CHAPTER IX
THE SURGICAL TREATMENT
The operative treatment of intervertebral disc lesions has acquired a poor reputation with the profession and with the public. Every patient on whom surgery is proposed seems to know someone who spent nine months in hospital after the operation, or who is worse than ever following spinal fusion, or who is paralyzed following the operation. It is not realized that he was probably paralyzed before the operation and may be making the notoriously slow and often incomplete recovery therefrom.
It often happens also that a confident diagnosis of a herniated intervertebral disc is made and then confirmed by finding the appropriate indentation of the dural tube on the myelogram.
However, at operation in a relaxed, unconscious patient in the prone position no herniation is seen. The posterior surface of the annulus appears to be normal. No other pathological process can be found, and the -wound is closed. The patient has endured a useless operation. The surgeon is downhearted and distressed. He may project his disappointment on to the patient and with good reason, from his point of view, may pronounce the patient a malingerer or neurotic - forgetting the confidence of his original diagnosis. The patient's disease proceeds unchecked in spite of the major operation. This is particularly unfortunate because if the surgeon had taken one small additional step the results would almost certainly have been good.
Operation is clearly indicated long before the nucleus herniates. However, cases continue to be seen in which the nucleus has herniated and in some of these signs of root, spinal cord, or cauda equina pressure, have been added to the previous symptoms. These are cases which have been neglected, no matter what the explanation may be and operation is necessary.
INDICATIONS FOR SURGERY
The indication for operation is failure after adequate treatment by traction and manipulation. From this trial we may conclude that the nucleus has worn through most of the posterior annulus and has become enmeshed in the eroded lamellae. In a few cases it will be found to have eased its way into the spinal canal.
It is a reasonable guess that a doctor in general practice sees about one case per two hundred cases of backache in which operation is indicated.
Orthopaedic surgeons see great numbers of patients with long histories of low back pain and have a much higher surgical rate.
Neurosurgeons to whom cases with demonstrable paralyses are likely to be referred are confronted with cases which are mostly surgical. They take great and misguided pains to prove that their patients are actually suffering from herniated discs.
The thinking of an individual in any of the above groups on backache is therefore likely to be considerably biased by his own experience.
The patients who come to operation have had a long history in the order of ten to fifteen years or more since their first attack of backache. One should remember to ask the patients on the first examination, and subsequently, how long it has been since the first attack of back pain of this type. They may have had many periods of acute exacerbations and incomplete remissions; and some will be found who have been disabled for practically the whole period.
The custom, and it seems to be universal, is for the orthopaedic surgeons to operate on their own patients with lumbar disc lesions. Since few dorsal or cervical disc lesions become surgical problems, and an individual orthopaedic surgeon does not see many of them, they are usually referred to a neurosurgeon who takes a particular interest in this problem. The same principles apply.
X-RAYS
X-Rays are not taken unless the diagnosis becomes in doubt or the decision has been made to operate on the patient. We take them routinely prior to myelogram to minimize the possibility of error.
MYELOGRAM
EDITOR'S NOTE: In modern times, myelography has largely been replaced by the less invasive CT and MRI technologies. The CT myelogram, however, may still be used in those cases where MRI technologies may not be employed, such as patients with implanted electronic devices such as pacemakers. The authors original text continues:
A myelogram is, not infrequently, a gruelling experience to the patient. Patients complain more about it than they do about the operation; and it has definite, even if slight, attendant dangers.
One is the accidental puncture of a normal nucleus which initiates another nuclear lesion. The second complication is rare, but it has occurred, and that is, the sudden development of a flaccid paraplegia, which is painfully slow in its progress to incomplete recovery. There is too, the slight danger of infection, which in practice is so small as to be only of academic importance. Statistically it is negligible, yet to the individual who has suffered such an infection it is the most shatteringly important single fact in his life. Myelograms must be done by, or closely supervised by, experts.
It has been demonstrated experimentally by Hirsch1 that a normal intervertebral disc can, with its component intervertebral bodies, one above and one below, withstand the pressure from a weight of 220 pounds with less than one milli-meter bulging of the annulus. The anterior surface of the dural tube is separated from the posterior surface of the annulus by fat, vessels and nerves and the posterior longitudinal ligament. The almost imperceptible bulging caused by this considerable weight would not register. Therefore, any indentation of the dural tube, or of the dural investment of the root, observed on the myelogram is significant, and when correlated with the clinical findings is conclusive. The conclusion that this is due to a nuclear lesion of the intervertebral disc is one of the most reliable judgments in the practice of medicine.
Confirmation by myelogram is a valuable reassurance to the surgeon; but the level of the lesion can be accurately located by the spinous process thrust test. A marker taped over this spinous process points exactly at the involved intervertebral disc in x-rays. If the surgeon has done a number of manipulative treatments prior to advising operation he will have found that it Is always the same spinous process. The myelograms constantly confirm this. If more than one intervertebral disc is involved, it will always be the same spinous processes. A confident surgeon can certainly proceed on the clinical information without having a myelogram done. Occasionally, though, he may be deceived by the presence of an unsuspected lesion or by another nuclear lesion in a neighbouring intervertebral disc.
THE OPERATION
The purpose of the operation is to remove completely the fibrous nucleus of the affected intervertebral disc whether it is herniated or not, while avoiding injury to the inner surface of the annulus.
The operation is not difficult for one accustomed to spinal surgery. It is only the removal of a foreign body, even if it is deeply placed. The approach through the midline of the back cuts nothing of importance and rapid recovery should be routine. The dangers are those common to all surgical operations. The surgeon's aseptic technique in this region must be particularly careful because the contents of the spinal canal are relatively defenseless, and the introduction of pyogenic bacteria is likely to be enormously destructive.
The patient is placed face down on bolsters on the operating table, or with firm pillows under the chest, and pelvis and proximal thighs, so that the abdomen hangs downward without any pressure upon it. This allows free drainage of the veins inside the vertebral canal via the numerous valveless anastomoses with the abdominal veins, and assures a relatively bloodless field within the spinal canal. In addition our anaesthetists instill a vasoconstrictor solution extradurally into the spinal canal prior to the operation.
The skin incision is in the mid-line of the back, about three inches long, its centre being over the distal tip of the spinous process of the vertebra above the affected intervertebral disc.
The soft tissues are divided down to the spinous processes. With a knife, the soft tissue over the spinous process of the vertebra above the nuclear lesion is incised vertically in the mid-line, down to bone. One of the lips so formed is then grasped in a strong forceps and the soft tissue is separated from the spinous process downwards and from the lamina laterally, by means of a broad periosteal elevator. The space thus obtained is firmly packed with a tail-sponge of convenient size (about 10" long by 2" wide). Firm packing at every step in the procedure controls bleeding and does most of the dissection.
The soft tissues attached to the other side of the spinous process and lamina are dealt with similarly, and the procedure is repeated at the spinous process and the lamina of the vertebra below.
The spinous processes are cut horizontally (Fig. 76) and retractors are inserted.
A small incision is made through the ligamentum flavum, which is now completely exposed. Care must be taken to avoid cutting the dura. There is space between the ligamentum flavum and the dura which is partially filled with epidural fat, so the danger is slight. Curved scissors, or a Kerrison forceps, are then used to cut and remove the ligamentum flavum between the two adjacent laminae.
Retraction of the dura exposes the nerve root, which is drawn aside, and carefully isolated with a root retractor. The nerve at the level of a low lumbar disc is almost straight up and down and it lies in front of the dural tube. The first sacral root at the level of L5 - S1 inclines more laterally than those immediately above. Sometimes it is more convenient to draw this root laterally while retracting the dura medially.
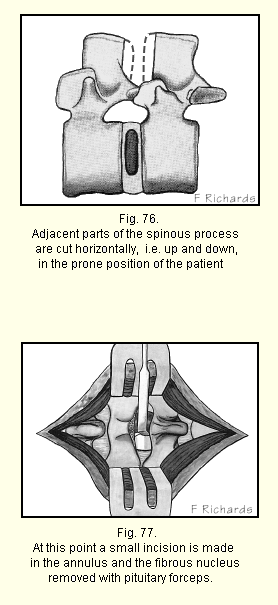
A good view of the posterior surface of the annulus lying immediately below is now obtained (Fig. 77). It is not necessary to remove any of the lamina unless the fibrous nucleus has herniated into the spinal canal and drifted downwards.
The field is kept dry by suction, sometimes assisted by small packs above and below. If there is no herniation or bulging of the annulus evident on inspection of each side after retraction of the dura, a quarter inch transverse incision is made in the annulus close to the posterior longitudinal ligament and the nucleus removed with pituitary forceps. It may come out in one piece or there may be a number of smaller pieces. All loose fragments are removed by exploring the inner surface of the nuclear space gently with a curette. One must be careful not to injure the inner surf ace of the annulus. To do so is likely to prepare further fragments for later extrusion.
If one should, in error, expose a normal nucleus, it is immediately evident. The pearly-greyish almost colourlesss jelly contrasts obviously with the pigmented fibrous tissue. If a normal nucleus has been exposed the nuclear jelly must be removed as completely as possible, because any mesenchyme left will turn to fibrous tissue and cause later trouble. This is a difficult task, but it is an error which, with ordinary precautions, should never occur.
After removing all packs, the muscles, fascia and skin are closed in the usual manner.
In this operation it is particularly easy to lose small sponges in the wound. If they have to be used long strings should be attached to them.
Since the approach has been made in the mid-line of the back across which there is no structure of importance, and only an irritating foreign body has been removed, no significant damage has been done. The results, as a rule, should be excellent.
We allow the patients up the next day and allow them to go home in four or five days.
It has been said that as the result of this operation fibrous union and eventually bony fusion occurs between the opposing vertebral bodies, but we do not believe there is any basis for this opinion. In a few cases in which we have had an opportunity to explore the same disc tong after the original operation, we have found no evidence of any such process.
The Swedish orthopaedic surgeons send their workmen back to heavy labour within a month, but in our experience workmen take a good deal longer than that, in spite of assurances that no activity is likely to do them any harm. Patients in less arduous occupations are able to return to work in a few weeks.
Superior patients obtain superior results. What can be achieved is shown by the case of a rugged, athletic middle-aged surgeon. His low back pain of twenty years' duration had run the usual course of acute exacerbations and incomplete remissions. For two years he had had radiation of pain running all the way down the left leg and into the toes. He was severely disabled. He obtained some relief from occasional treatments by traction and manipulation. He was told that excision of the nucleus of the L 4-5 disc was indicated and probably unavoidable, but somehow, he managed to continue working for another year. One afternoon, he appeared with a dropped left foot. There was no sensory change in the foot or elsewhere in the leg. He was booked for surgery.
At operation the fibrous nucleus was found to have partly extruded into the spinal canal. It lay under (i.e. anterior to) the nerve, but in the prone position of the patient, did not seem to be exerting any pressure on it. When visited the next morning, the patient was walking around his room. Full motion had returned to the dropped foot. He had voided and passed flatus. He had needed no medication and declared himself ready to leave the hospital. He was dissuaded with some difficulty, but he left the next morning. On the seventh post-operative day be went water skiing and played a round of golf. He has since taken care of his large surgical practice without a pause.
In my opinion, spinal fusion has little or no place in the treatment of nuclear lesions of intervertebral discs, and certainly none prior to the excision of the fibrous nucleus. However, Cloward who pioneered the anterior approach to the intervertebral discs in the cervical spine, firmly believes that interbody spinal fusion must be done in his cases2.
We do not give blood to patients who undergo surgery for excision of a vertebral nucleus. These patients are in good health and can easily stand a blood loss of 300 or 400 cc. This loss is much reduced by the instillation of a vasoconstrictor solution into the spinal canal.
Since the publication of R. Campbell Begg's3 article on postoperative gaseous distension in 1948 many Vancouver surgeons have followed his advice. It is based on the fact that following operations or other injuries of sufficient severity peristalsis ceases for a period varying from hours to many days. Its absence is determined by auscultation. During that period it is unwise to allow the patient to swallow anything but his own saliva. Mr. Begg points out that air swallowing is not a factor in distension. For example, it is not applicable in lightning stroke, renal colic, anuria and so forth unless one is to suppose that the victims suddenly become addicts of air swallowing. Further, to tie off or cut the oesophagus in animal experiments is the equivalent of giving nothing by mouth.
If a small suction tube is kept in the stomach it is not that the tube removes swallowed air but that it keeps the stomach empty and thus neutralizes the effects of introduced fluids. If fluids or food reach the stomach during the refractory period they cause this organ to contract on its contents, leading to a reflex reduction in tone in the intestine. This enables gas, available from bowel capillaries, to flow in to fill the increased space in the lumen. The process of distension so commenced is irreversible until the spontaneous resumption of active peristalsis. The gas pains thus induced are distinctly unpleasant and are debilitating to the patient. Meteorism and adynamic ileus are dangerous. All fluids and medications are given either intravenously or hypodermically. When peristalsis has spontaneously resumed, its completion is signalled by the expulsion of flatus per rectum.
Patients who have had spinal surgery are subject to gaseous distension. Our experience confirms that rigid observance of the rule "nothing by mouth and no enemas" until flatus has been passed contributes a great deal to the comfort and safety of the patient.